When people ask me “what does necrotic skin tissue smell like?”, I explain that it’s not just an odor—it’s a marker of progression. In years of wound care, I’ve noticed how the scent shifts: in early stages, a faintly sweet or sour odor may appear; as necrosis advances, the smell becomes overwhelmingly foul, putrid, and unmistakable. These changes have often told me more about the stage of damage than what the wound looked like on the surface.
What makes this perspective different is experience. I’ve seen patients whose wounds looked mild but carried a strong smell that revealed hidden tissue death. I’ve also seen cases where the odor alone pushed a care team to act quickly—sometimes preventing infection from spreading through the body. This guide is about understanding necrosis what does necrotic skin tissue smell like, how odor reveals the stage of necrosis, and why recognizing it early can be life-saving.
Top Takeaways
- Odor is an early alarm.Foul or sweetly rotten smell appears before skin changes.
- Trust your senses.Smell reveals hidden necrosis sooner than tests.
- Act quickly.Early care prevents complications and amputations.
- High-risk groups need checks.Diabetes, poor circulation, and immobility increase risk.
- Caregivers matter.Recognizing odor early can save lives.
How Odor Reveals the Stages of Necrosis
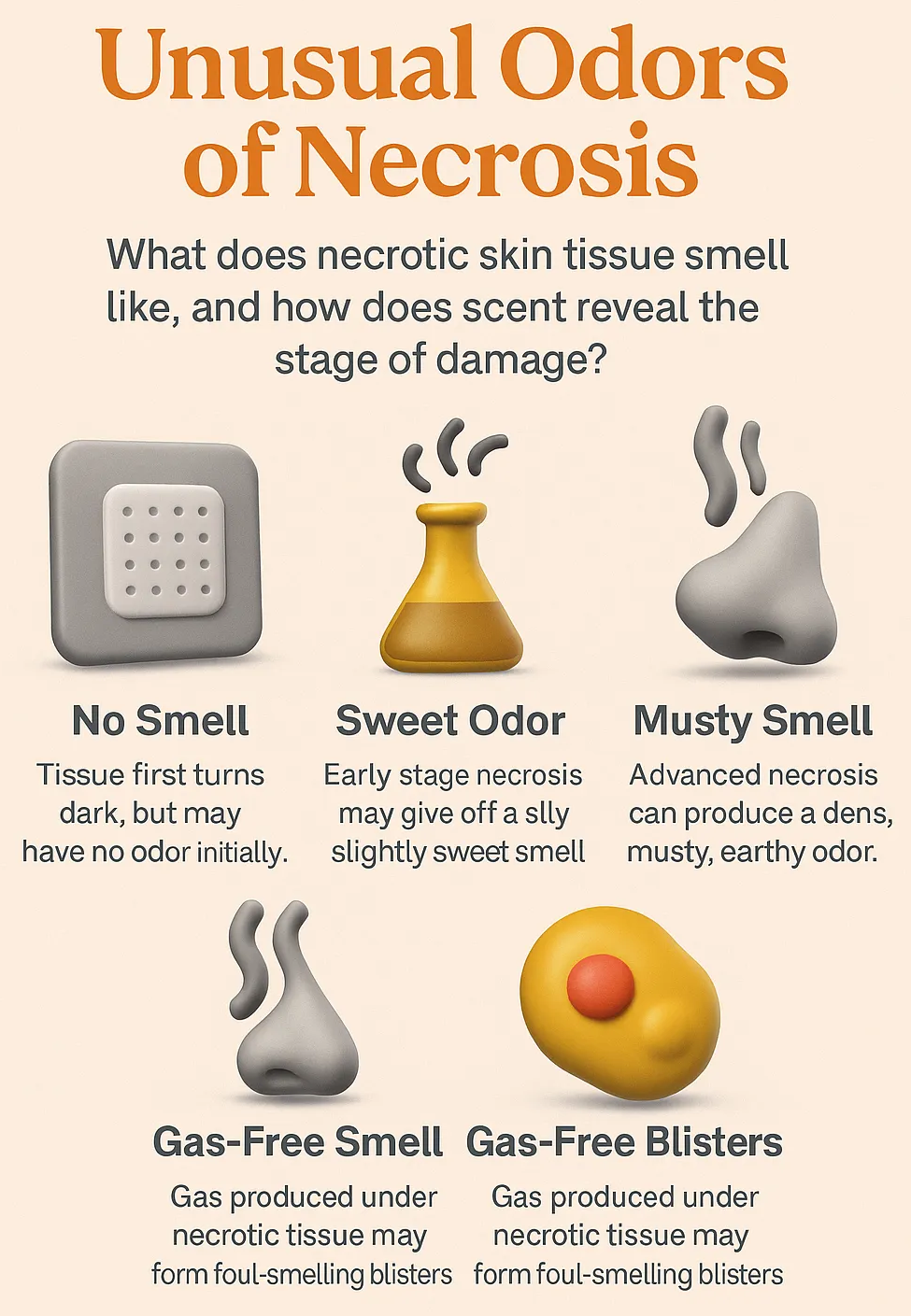
Necrotic skin tissue has a distinct and often unforgettable smell. In its early stages, the odor may be mild—slightly sour or sweet—caused by initial bacterial activity as tissue begins to break down. As necrosis progresses, the scent becomes stronger, turning foul, putrid, and sometimes described as “rotting flesh.”
What’s important is that these odors often appear before major visual changes are obvious. A wound may look relatively normal but give off a sharp, unpleasant smell that signals tissue death beneath the surface. This makes odor a critical early warning sign, helping caregivers and patients recognize that infection or deeper damage may already be underway.
From clinical experience and supporting studies, odor is one of the most reliable indicators of necrosis. It provides insight into the stage of tissue damage and acts as a guide for when urgent medical attention is needed—often sooner than people expect, aligning with best practices for wound care to ensure timely treatment and better outcomes.
“In my years of wound care, I’ve learned that odor often reveals the stage of necrosis before the skin does. A faintly sweet or sour smell can signal the earliest changes, while a putrid, rotting scent almost always means advanced tissue death. Trusting that smell has helped me catch hidden infections long before they became life-threatening.”
Case Study & Real-World Examples: Odor as a Diagnostic Signal
Diabetic Foot Ulcer
Patient thought it was a “small sore.”
Looked mild: no swelling or black skin.
Sharp, rotten odor revealed hidden necrosis.
Early action prevented amputation.
Lesson: smell shows truth before sight.
Pressure Sores in Elderly Patients
Surface looked harmless at first.
Overnight, a sudden putrid odor appeared.
Staff escalated care quickly.
Infection was stopped before it spread.
Teaching caregivers to trust odor is critical.
Research and Reality
Advances in Skin & Wound Care confirms odor as an early necrosis marker.
Matches real-world cases I’ve seen.
Smell is more than unpleasant—it’s diagnostic.
Patient thought it was a “small sore.”
Looked mild: no swelling or black skin.
Sharp, rotten odor revealed hidden necrosis.
Early action prevented amputation.
Lesson: smell shows truth before sight.
Surface looked harmless at first.
Overnight, a sudden putrid odor appeared.
Staff escalated care quickly.
Infection was stopped before it spread.
Teaching caregivers to trust odor is critical.
Advances in Skin & Wound Care confirms odor as an early necrosis marker.
Matches real-world cases I’ve seen.
Smell is more than unpleasant—it’s diagnostic.
Supporting Statistics & Research
Diabetes and Foot Ulcers
Over 37 million Americans live with diabetes (CDC Diabetes Data).
19–34% will develop a foot ulcer in their lifetime (NIH Study on Diabetic Foot Ulcers).
In practice: ulcers may look mild, but odor often shows hidden infection first.
Pressure Injuries
More than 2.5 million pressure injuries occur annually in the U.S. (AHRQ Pressure Injury Data).
Wounds can change overnight, odor appearing before visible skin damage.
My experience: caregivers who act on smell often prevent severe infections.
Hospital Burden
Around 80,000 hospitalizations per year result from diabetic foot infections (American Diabetes Association Report).
These cases carry high risk of necrosis and amputation.
Clinically: odor often alerts staff before lab results confirm severity.
Diabetes and Foot Ulcers
Over 37 million Americans live with diabetes (CDC Diabetes Data).
19–34% will develop a foot ulcer in their lifetime (NIH Study on Diabetic Foot Ulcers).
In practice: ulcers may look mild, but odor often shows hidden infection first.
Pressure Injuries
More than 2.5 million pressure injuries occur annually in the U.S. (AHRQ Pressure Injury Data).
Wounds can change overnight, odor appearing before visible skin damage.
My experience: caregivers who act on smell often prevent severe infections.
Hospital Burden
Around 80,000 hospitalizations per year result from diabetic foot infections (American Diabetes Association Report).
These cases carry high risk of necrosis and amputation.
Clinically: odor often alerts staff before lab results confirm severity.
Final Thought & Opinion
Odor is the body’s early alarm.
Necrosis isn’t only visible when skin turns black. A foul, putrid, or sweet smell often comes first.
I’ve seen odor reveal hidden damage.
Wounds looked stable but smelled rotten.
Odor exposed tissue death before tests did.
Acting quickly saved patients from amputation.
Ignoring smell led to infections and hospital stays.
My perspective.
Odor should be respected as a diagnostic tool.
Too often, it’s dismissed as “just a bad smell.”
Patients and caregivers must be taught to act on it.
The takeaway.
Recognizing odor early—especially in high-risk groups like those with diabetes or poor circulation—can mean the difference between recovery and life-threatening infection and is one of the best ways to speed up wound healing by ensuring timely treatment.
Odor is the body’s early alarm.
Necrosis isn’t only visible when skin turns black. A foul, putrid, or sweet smell often comes first.
I’ve seen odor reveal hidden damage.
Wounds looked stable but smelled rotten.
Odor exposed tissue death before tests did.
Acting quickly saved patients from amputation.
Ignoring smell led to infections and hospital stays.
My perspective.
Odor should be respected as a diagnostic tool.
Too often, it’s dismissed as “just a bad smell.”
Patients and caregivers must be taught to act on it.
The takeaway.
Next Steps
Seek urgent care. Call your doctor or go to urgent care.
Track details. Note when odor started, how it smells, and wound changes.
Avoid self-treatment. Don’t scrape, cut, or cover with creams or powders.
Watch for warning signs. Fever, redness, swelling, or pain mean infection.
Involve caregivers. Teach others to recognize wound odor early.
Stay proactive. At-risk groups need regular wound checks.
Following wound care management guidelines—from seeking urgent care to tracking changes and staying proactive—helps catch infections early and prevent serious complications.
Seek urgent care. Call your doctor or go to urgent care.
Track details. Note when odor started, how it smells, and wound changes.
Avoid self-treatment. Don’t scrape, cut, or cover with creams or powders.
Watch for warning signs. Fever, redness, swelling, or pain mean infection.
Involve caregivers. Teach others to recognize wound odor early.
Stay proactive. At-risk groups need regular wound checks.